Dysautonomia and the Neuroimmune Axis: Diagnosis and Management
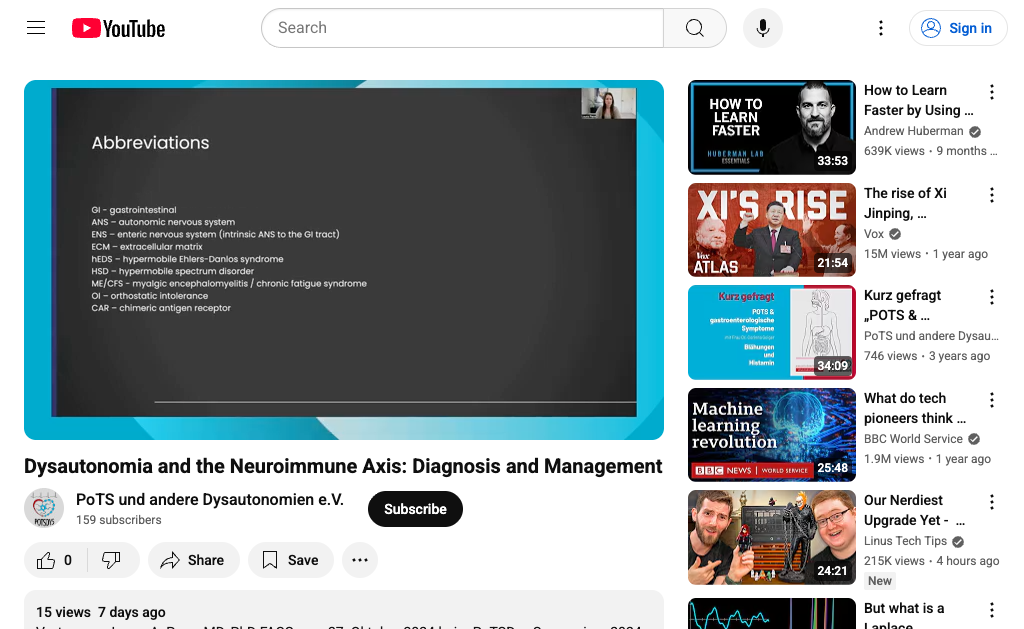
Dr. Laura A. Pace reviews how the neuroimmune axis—interactions between the autonomic nervous system and immune cells (including mast cells and neuroinflammation)—can drive dysautonomia presentations such as POTS, with frequent overlap with MCAS and hypermobility/EDS. She emphasizes careful phenotyping and differential diagnosis, outlining practical evaluation steps (history, orthostatic vitals/tilt testing, heart rate variability and sudomotor assessments where available, GI and other organ-specific testing as indicated, and targeted labs to identify immune activation or secondary causes). Management focuses on treating the underlying drivers (e.g., addressing inflammation, infections, autoimmune features, and GI dysfunction), alongside core dysautonomia care: volume expansion (fluids/salt), compression, posture and activity modification/pacing, sleep optimization, nutrition, and graded, symptom-informed conditioning. Pharmacologic options are individualized and may include medications for heart rate/blood pressure control, antihistamines and mast-cell–directed therapies when MCAS features are present, and agents targeting pain, GI motility, and neuroimmune symptoms. She highlights multidisciplinary coordination, patient education, and monitoring over time, as symptom clusters and triggers can evolve.